OSTEOARTHRITIS
Overview
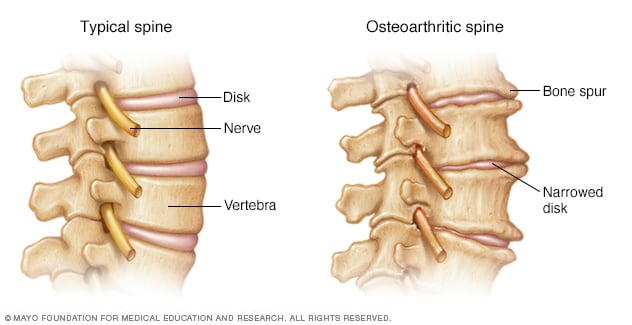
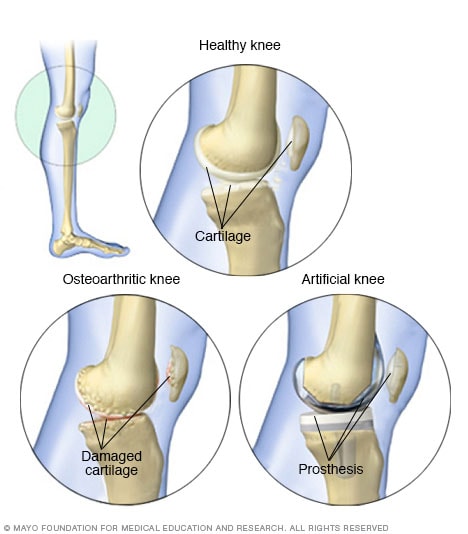
Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of your bones wears down over time.
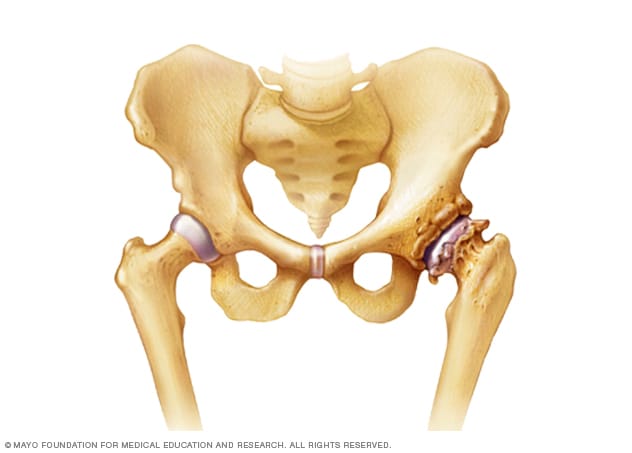
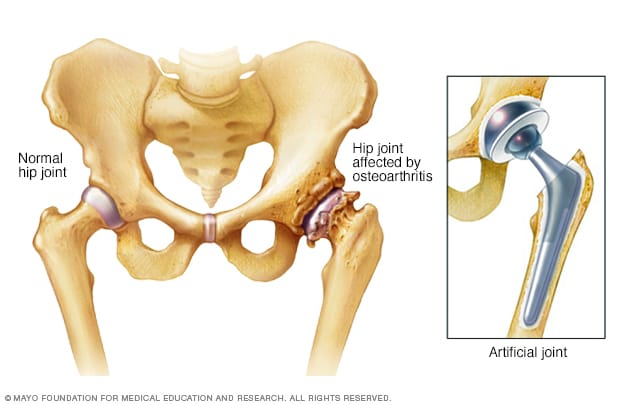
Although osteoarthritis can damage any joint, the disorder most commonly affects joints in your hands, knees, hips, and spine.
Osteoarthritis symptoms can usually be managed, although the damage to joints can't be reversed. Staying active, maintaining a healthy weight and some treatments might slow the progression of the disease and help improve pain and joint function.
Symptoms
Osteoarthritis symptoms often develop slowly and worsen over time. Signs and symptoms of osteoarthritis include:
- Pain. Affected joints might hurt during or after movement.
- Stiffness. Joint stiffness might be most noticeable upon awakening or after being inactive.
- Tenderness. Your joint might feel tender when you apply light pressure to or near it.
- Loss of flexibility. You might not be able to move your joint through its full range of motion.
- Grating sensation. You might feel a grating sensation when you use the joint, and you might hear popping or crackling.
- Bone spurs. These extra bits of bone, which feel like hard lumps, can form around the affected joint.
- Swelling. This might be caused by soft tissue inflammation around the joint.
causes
Primary causes- unknown
Secondary cause-
1. Joint trauma
2. Prior inflammatory arthritis, example -gout, rheumatoid arthritis,
3. Metabolic disorder
4. Endocrinal disorder (diabetes, acromegaly)
5. Collagen defect
6. Others (osteoporosis)
- Heredity. Some people have an inherited defect in one of the genes responsible for making cartilage. ...
- Obesity. Obesity increases the risk of osteoarthritis of the knee, hip, and spine. ...
- Injury. Injuries contribute to the development of osteoarthritis. ...
- Joint overuse. ...
- Other diseases.
Risk factors
Factors that can increase your risk of osteoarthritis include:
- Older age. The risk of osteoarthritis increases with age.
- Sex. Women are more likely to develop osteoarthritis, though it isn't clear why.
- Obesity. Carrying extra body weight contributes to osteoarthritis in several ways, and the more you weigh, the greater your risk. Increased weight adds stress to weight-bearing joints, such as your hips and knees. Also, fat tissue produces proteins that can cause harmful inflammation in and around your joints.
- Joint injuries. Injuries, such as those that occur when playing sports or from an accident, can increase the risk of osteoarthritis. Even injuries that occurred many years ago and seemingly healed can increase your risk of osteoarthritis.
- Repeated stress on the joint. If your job or a sport you play place repetitive stress on a joint, that joint might eventually develop osteoarthritis.
- Genetics. Some people inherit a tendency to develop osteoarthritis.
- Bone deformities. Some people are born with malformed joints or defective cartilage.
- Certain metabolic diseases. These include diabetes and a condition in which your body has too much iron (hemochromatosis).
Complications :
- A rapid, complete breakdown of cartilage resulting in loose tissue material in the joint (chondrolysis).
- Bone death (osteonecrosis).
- Stress fractures (hairline crack in the bone that develops gradually in response to repeated injury or stress).
- Bleeding inside the joint.
Diagnosis
During the physical exam, your doctor will check your affected joint for tenderness, swelling, redness and flexibility.
Imaging tests
To get pictures of the affected joint, your doctor might recommend:
- X-rays. Cartilage doesn't show up on X-ray images, but cartilage loss is revealed by a narrowing of the space between the bones in your joint. An X-ray can also show bone spurs around a joint.
- Magnetic resonance imaging (MRI). An MRI uses radio waves and a strong magnetic field to produce detailed images of bone and soft tissues, including cartilage. An MRI isn't commonly needed to diagnose osteoarthritis but can help provide more information in complex cases.
Lab tests
Analyzing your blood or joint fluid can help confirm the diagnosis.
- Blood tests. Although there's no blood test for osteoarthritis, certain tests can help rule out other causes of joint pain, such as rheumatoid arthritis.
- Joint fluid analysis. Your doctor might use a needle to draw fluid from an affected joint. The fluid is then tested for inflammation and to determine whether your pain is caused by gout or infection rather than osteoarthritis.
Treatment
Osteoarthritis can't be reversed, but treatments can reduce pain and help you move better.
Medications
Medications that can help relieve osteoarthritis symptoms, primarily pain, include:
- Acetaminophen. Acetaminophen (Tylenol, others) has been shown to help some people with osteoarthritis who have mild to moderate pain. Taking more than the recommended dose of acetaminophen can cause liver damage.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Over-the-counter NSAIDs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve, others), taken at the recommended doses, typically relieve osteoarthritis pain. Stronger NSAIDs are available by prescription.NSAIDs can cause stomach upset, cardiovascular problems, bleeding problems, and liver and kidney damage. NSAIDs as gels, applied to the skin over the affected joint, have fewer side effects and may relieve pain just as well.
- Duloxetine (Cymbalta). Normally used as an antidepressant, this medication is also approved to treat chronic pain, including osteoarthritis pain.
Therapy
- Physical therapy. A physical therapist can show you exercises to strengthen the muscles around your joint, increase your flexibility and reduce pain. Regular gentle exercise that you do on your own, such as swimming or walking, can be equally effective.
- Occupational therapy. An occupational therapist can help you discover ways to do everyday tasks without putting extra stress on your already painful joint. For instance, a toothbrush with a large grip could make brushing your teeth easier if you have osteoarthritis in your hands. A bench in your shower could help relieve the pain of standing if you have knee osteoarthritis.
Surgical and other procedures
If conservative treatments don't help, you may want to consider procedures such as:
- Cortisone injections. Injections of corticosteroid medications may relieve pain in your joint. During this procedure, your doctor numbs the area around your joint, then places a needle into space within your joint and injects medication. The number of cortisone injections you can receive each year is generally limited to three or four injections because the medication can worsen joint damage over time.
- Lubrication injections. Injections of hyaluronic acid may offer pain relief by providing some cushioning in your knee, though some research suggests these injections offer no more relief than a placebo. Hyaluronic acid is similar to a component normally found in your joint fluid.
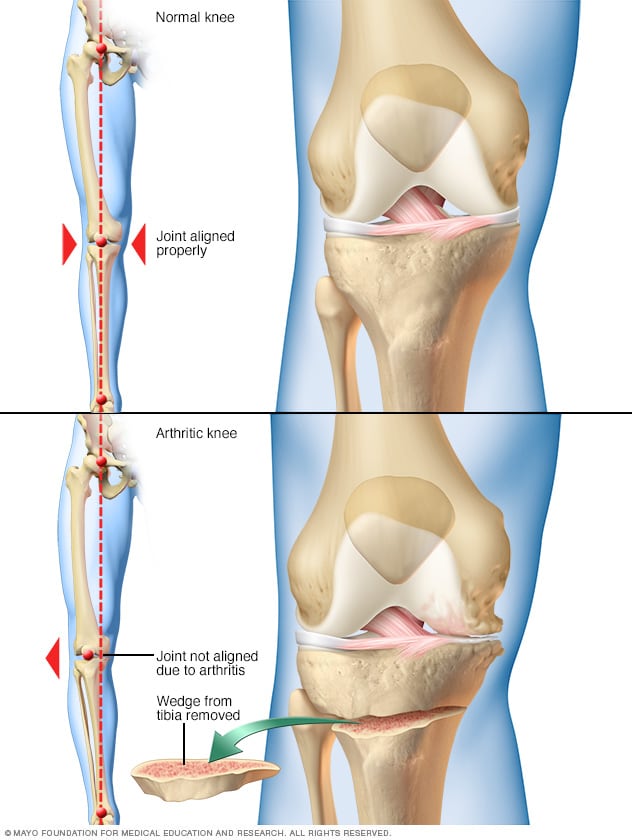
- Realigning bones. If osteoarthritis has damaged one side of your knee more than the other, an osteotomy might be helpful. In a knee osteotomy, a surgeon cuts across the bone either above or below the knee, and then removes or adds a wedge of bone. This shifts your body weight away from the worn-out part of your knee.
- Joint replacement. In joint replacement surgery (arthroplasty), your surgeon removes your damaged joint surfaces and replaces them with plastic and metal parts. Surgical risks include infections and blood clots. Artificial joints can wear out or come loose and may need to eventually be replaced.
QUESTIONS SERIES???????????
1. What is the best treatment for osteoarthritis?
- Acetaminophen. Acetaminophen (Tylenol, others) has been shown to help some people with osteoarthritis who have mild to moderate pain. ...
- Nonsteroidal anti-inflammatory drugs (NSAIDs). ...
- Duloxetine (Cymbalta).
2. What are the 4 stages of osteoarthritis?
Arthritis in Knee: 4 Stages of Osteoarthritis
- Stage 0- Normal. When the knee shows no signs of osteoarthritis, it is classified as Stage 0, which is normal knee health, with no known impairment or signs of joint damage. ...
- Stage 1- Minor. ...
- Stage 2-Mild. ...
- Stage 3- Moderate. ...
- Stage 4- Severe.
3. What is the main cause of osteoarthritis?

















%20(1).jpeg)
%20(1).jpeg)